|
This article is a continuation of: The aortic root and the aortic valve (1) The aortic valve is formed by three semilunar leaflets which are very thin as to be almost transparent. The attachment of the leaflets is complex, as part of them attaches to ventricular wall, part attaches to the sinusal arterial wall, and even part of them attaches to the membranous interventricular septum and other fibrous structures. Loukas et al state that at “least one third of the circumference of the aortic root is supported by fibrous tissue rather than ventricular musculature” Each of the three aortic leaflets has a semilunar attachment and shape (hence the term “semilunar valve” used for both the aortic and pulmonary valve, as they have similar shape). The attachment of these three leaflets create a continuous line where the highest points are the three locations where the leaflets attach at the STJ, and the three lower points or “nadirs” form an edge shaped like a three-pronged “coronet”. This coronet is called by many the “anatomical anulus” of the aortic valve, as this is where the fibrous skeleton of the heart forms the “hinges” of the aortic valve. |
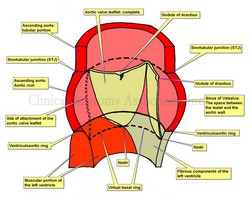 Aortic root and aortic valve. Click on the image for a larger version. |
| The leaflets of the aortic valve (as well as those in the pulmonary valve) have a tissue excrescence that can become quite hard at the point where the three leaflets touch on each heartbeat. These are the nodules of Arantius, named after Giulio Cesare Aranzio (1530 – 1589). As a side note, the nodules of the pulmonary valve have a different name. Distally, the aortic leaflets may present a very thin extension that may be cribriform (not shown in the sketch). These are called the lunulae (singular: lunula) as they look like a sliver of moon.
The second component of the base of the aortic root is a ring defined by the lowest portion of each leaflet, the nadir. This ring is called the “virtual basal ring”, is found within the left ventricle and is used as a surgical reference for aortic valve replacement implants. The three leaflets are found within three dilations of the aortic root, each one called a “sinus of Valsalva”, which extend between the virtual basal ring inferiorly and the STJ superiorly. The presence of the sinuses of Valsalva permits “fluttering” of the open aortic leaflets in ventricular systole. This fluttering of the leaflets allows blood to flow into the sinuses and into the coronary arteries during ventricular systole. Aortic valve may present with different number of leaflets, as in the case of a bicuspid aortic valve. The shape of the attachment of the leaflets create two distinct situations: First, there is a portion of the ventricle related to the leaflets where the ventricle acts as an artery, the aorta. These areas are found inside the sinuses of Valsalva. Second, there are triangular areas of the aortic root (the interleaflet triangles) where the aortic wall is within the left ventricle and submitted to the pressures and hemodynamics of the left ventricle. These interleaflet triangles have been involved in aneurysms. For simplicity, these interleaflet triangles are not shown in the sketch and are the subject of a separate article in this website. Note: The image depicts only one complete aortic leaflet. The other one has been transected to show the sinus of Valsalva and the third has been removed to show the attachment or "hinge" of the leaflet. For an anatomical image of the aortic valve click here. Sources: |
|
| MTD Main Page | Subscribe to MTD |