Cerebelum
The word [cerebellum] is Latin and means "little brain". The cerebellum is one of the three main gross components of the brain (encephalon), the other two being the cerebral hemispheres and the brain stem.
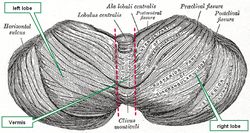
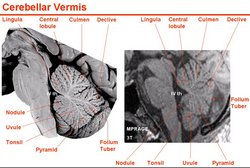
The cerebellum is characterized by a tightly folded external cortex where the gyri are long and parallel to each other and the sulci are not very deep. Upon gross examination, the cerebellum presents with two lateral lobes (left and right) and a median lobe known as the vermis. Other authors divide the cerebellum into an anterior and posterior lobe separated by a primary fissure or sulcus, also known as the preclival sulcus.
Cerebellar vermis
The cerebellum is located posterior to the brain stem and posteroinferior to the cerebral hemispheres. It is separated from the occipital lobes of the brain by an extension of dura mater called the tentorium cerebelli. Because of its location, the cerebellum serves as a roof for the 4th ventricle, a component of the ventricular system of the brain. Click here to see a median section, of the cerebellum where you can observe its location and relation to the brain stem, 4th ventricle, and occipital lobe.
The cerebellum is part of the motor control of the brain and is involved in motor coordination, precision, balance and accurate motor timing. Cerebellar dysfunction does not cause paralysis, but produces fine motor control disorders.
Median section image link courtesy of UCLA Radiology.
Sources:
1 "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
2. "Anatomy of the Human Body" Henry Gray 1918. Philadelphia: Lea & Febiger
Image modified by CAA, Inc. Original image courtesy of bartleby.com