| About 30 million people worldwide carry an AFib diagnosis. Today seems everyone either has AFib or knows someone that has AFib. When I first held an Afib seminar in Beijing, China, over 1200 people with AFib signed up for the seminar. It was standing room only!
Despite the common occurrence of AFib around the world, a recent study found that in patients who were diagnosed with AFib, 40-50% of patients with an elevated risk of stroke were not treated with the best therapy, and the rate of stroke over the next five years was 10%.
Here in Houston, we can do better! Learn more about AFib right here today, and I guarantee you will have hope and be more likely to reach your goal of feeling better.
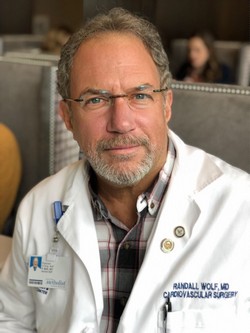
Towards an AFib free healthy life,
Randall K. Wolf, MD.
SEMINAR AGENDA
9:00 am Introductions - Randall Wolf, MD, FACS, FACC, Professor at McGovern Medical School, Cardiothoracic Surgery, Course Director for the AFib Patient Experience Seminar
9:15 am The cost of AFib
9:30 am Mechanisms
9:45 am Blood Thinners – W. Ross Brown, MD, FACC, Comprehensive Heart Care, PA
10:15 am Medications – Sunil Reddy, MD, Assistant Professor at McGovern Medical School, Cardiovascular Medicine
10:30 am BREAK
10:45 am Diet – Baxter Montgomery, MD, FACC, Clinical Assistant Professor of Medicine, McGovern Medical School, Department of Cardiology
11:00 am Sleep Apnea – Murtuza Ahmed, MD, FAASM, Razzack and Associates, Houston
11:15 am AF Monitoring – Sunil Reddy, MD, Assistant Professor at McGovern Medical School, Cardiovascular Medicine
11:30 am Questions with panel
12 noon LUNCH
Testimonials: Donna Roth, Houston, TX Gary Wight, Houston, TX Mac Peirson, Houston, TX Ross Wroblewski, Lompac, CA Michaela Senk-Eustace, Hartford, CT
1:00 pm Catheter Ablation – Siddharth S. Mukerji, MD, Assistant Professor at McGovern Medical School, Cardiovascular Medicine
1:30 pm Surgery – Randall Wolf, MD, FACS, FACC
2:00 pm Stop AFib.org – Mellanie True Hills, President
2:30 pm Panel Discussion
2:45 pm Stroke – Ritvij Bowry, MD, Assistant Professor at McGovern Medical School, Vivian L. Smith Department of Neurosurgery
3:00 pm LAA Closure – Siddharth S. Mukerji, MD, Assistant Professor at McGovern Medical School, Cardiovascular Medicine & Randall Wolf, MD, FACS, FACC
3:30 pm Panel Discussion
4:00 pm Adjourn – Meet with Faculty
ABOUT THE HOUSTON AFIB PATIENT EXPERIENCE SEMINAR
The University of Texas McGovern Medical School, Cardiothoracic and Vascular Surgery Department in Houston, is proud to host the inaugural Houston AFIB Patient Experience Seminar. The purpose is to educate the public in an interactive format allowing the audience to engage in conversation in a question/answer format with leading medical professionals. Our list of panel members and guest presentations include surgeons, cardiologists, neurologists, pulmonologists as well as testimonials from AFib patients. We are honored to be able to bring awareness to the resources and options available to patients suffering from AFIB.
NOTE: If you cannot attend the seminar, there is more information on Atrial Fibrillation at this website; click here.
|



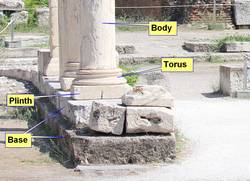
![Torus - By LucasVB [Public domain], via Wikimedia Commons](/images/MTD/SmallImages/torus_sm.jpg)