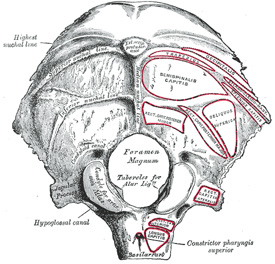
External view of the occipital bone
The term [inion] is Greek [ινιον] and originally referred to the posterior aspect of the neck or occiput and its musculature and strength, as mentioned in the Iliad.
The term fell in disuse for hundreds of years, until it was resurrected by Peter Paul Broca (1824-1880) as a craniometric point. The inion is the midline protuberance in the posteroinferior aspect of the external surface of the occipital bone. Today, in most anatomy texts the inion is referred to as the "external occipital protuberance"
The inion is found at the intersection of three bony lines that are easily palpable, the bilaterally situated superior nuchal line, and the median nuchal line. It is labeled "Ext. occip. protuberance" (see accompanying image). There is a corresponding internal occipital protuberance in the internal aspect of the occipital bone.
Sources:
1. "The Origin of Medical Terms" Skinner, HA 1970 Hafner Publishing Co.
2. "Medical Meanings - A Glossary of Word Origins" Haubrich, WD. ACP Philadelphia
3 "Tratado de Anatomia Humana" Testut et Latarjet 8 Ed. 1931 Salvat Editores, Spain
4. "Anatomy of the Human Body" Henry Gray 1918. Philadelphia: Lea & Febiger
Image modified by CAA, Inc. Original image by Henry Vandyke Carter, MD., courtesy of bartleby.com