|
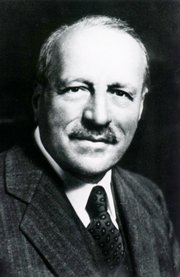
George Papanicolau, MD, PhD (1883 - 1962) Greek physician, cytologyst, physyiologist, and zoologist, Papanicolaou was born on the island of Euboea, Greece. His original Greek name is Georgios Nikolaou Papanikolaou. He initially attended the University of Athens, earning his MD in 1904.
After two years as a conscript in the Army, Papanicolaou continued additional studies in Zoology earning his PhD in 1910, later going back to the army as a physician.
Papanicolaou immigrated to the USA in 1913 with his wife. He took a position at the anatomy department of the Cornell University where over the next 45 years established the field of diagnostic cytology, becoming a Professor Emeritus of Clinical Anatomy.
His studies took him to study the cytological patterns in the internal genitalia of guinea pigs, establishing a “cytological calendar”. This study he continued in humans, where he discovered malignant changes in some of the cells obtained. His study on vaginal smears was published in 1943, starting what today is known as a “Pap smear”, a simple annual study that saves thousands of women from cervical and uterine cancer.
Dr. Papanicolaou died in 1960. His personal motto was “I live to serve life”
|
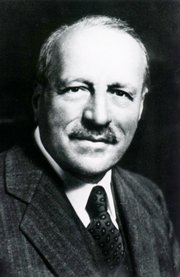 Original image courtesy of www.nih.gov Original image courtesy of www.nih.gov |
Sources:
1. “George Nicholas Papanicolaou, 1883-1962” Owens, C. Endoc T 2008:6(5) 28
2. "George N Papanicolaou (1883-1962) MD" Frangos, CC. J Me Biog 17 (3) 134
3. "George N. Papanicolaou, MD, PhD" Elgert, P A; Lab Med (2009) 40;4 245
4. "The diagnostic value of vaginal smears in carcinoma of the uterus" Papanicolaou, GN; Traut HF; Amm J Obst Gyn 1941; 42:193-206. |

![Fossa Ovalis [A]](http://farm8.staticflickr.com/7160/6450580573_2d18c738ed_z.jpg)
 Original image
Original image