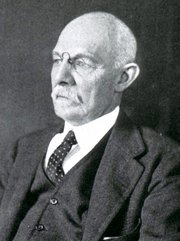
This article is part of the series "A Moment in History" where we honor those who have contributed to the growth of medical knowledge in the areas of anatomy, medicine, surgery, and medical research.

Ephraim McDowell
Ephraim McDowell (1771- 1830). American surgeon, Ephraim McDowell was born in 1771 in the Augusta County of Virginia. His family moved to the “frontier”, which at that time was Kentucky, where his father was a judge. McDowell studied in Kentucky and returned to Virginia to serve as an apprentice to Dr. Alexander Humphreys. Following Dr. Humphrey’s advice McDowell went to Edinburgh to finish his formal medical training, which he did not finish, taking chemistry, anatomy, and then a private medical course with Dr. John Bell.
Returning to America, he settled in the Ohio River Valley, and had a successful practice as a frontier surgeon in the city of Danville, Kentucky. This was before the advent of anesthesia and antisepsis.
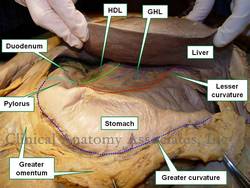
On Christmas Day 1809, Dr. McDowell performed the first recorded ovariotomy to drain a massive ovarian cyst from Mrs. Mary Jane Crawford, who had to ride a horse for sixty miles to get to Dr. McDowell’s office where he performed the ovariotomy without anesthesia. Mrs. Crawford had been diagnosed as “pregnant” by two other physicians. Dr. McDowell’s hand-written report states that he performed a nine-inch abdominal incision, the operation lasted about twenty five minutes, and they removed “fifteen pounds of a dirty gelatinous substance” and “extracted the sac, which weighed seven and a half pounds”.
Mrs. Crawford survived the operation, was ambulatory in five days, and lived for 33 additional years, until she was 78 years old. Research has been made as to the reason for the survival at a time when the norm for an operation that penetrated the peritoneal cavity was death. Othersen (2004) states that his research indicated that Dr. McDowell was “meticulous, neat and scrupulously clean”.
Because of the times, and because Dr. McDowell was not into writing, the achievement was not known for many years, until 1817. Dr. McDowell later performed a lithotomy on James Polk, who would eventually become president of the United States. In 1825, his achievements were recognized and he received an honorary MD degree by the University of Maryland.
Dr. McDowell’s house in Danville, KY is today a museum, and his name is remembered by the “Ephraim McDowell Health System” a group of integrated healthcare based in the same city. For more information on Mary Jane Crawford, click here.
PERSONAL NOTE: On February 19, 2017 I was able to go visit this place. Click here for a series of articles and pictures of this visit. Dr. Miranda
Sources:
1. “Ephraim McDowell (1771-1830) Kentucky Surgeon” JAMA. 1963;186 (9):861-862
2. “Ephraim McDowell: The Qualities of a Good Surgeon” Othersen, HB Ann Surg. 2004; 239(5): 648–650
3. “Ephraim McDowell (1771-1830): pioneer of ovariotomy” Tan,SY & Wong, C. Singapore Med J 2005; 46(1) : 4
4. “Ephraim McDowell, the First Ovariotomy, and the Birth of Abdominal Surgery” Horn, L and Johnson, DH. J Clin Onco 2010: 28; 7 1262-1268
5. "Surgeon of the wilderness: Ephraim McDowell" Haggard, WD. Presidential Address, ACS 1933. FACS archives 1934, 58: 415-4198
Image in Public Domain. Courtesy of the National Library of Medicine.