|
Leonardo Botallus (c.1530- ??) Italian anatomist and physician,Leonardo Botallus (also known as Botalli, Botallo, or Botal) was born circa 1530 in the region of Piedmont. Botallus studied medicine at the italian university of Pavia, where he was a student under Gabrielle Fallopius. Botallus graduated circa 1553. He was an avid advocate of bloodletting, causing him to direct his anatomical studies towards the subject of the vascular system. Although he did not discover the foramen ovale and the ductus arteriosus, he mentions these structures by those names in both his posthumous publications " De via sanguinis a dextro in sinistro cordis ventriculum" (1640) and "Opera Omnia Medica et Chirurgica" (1660)
In France Botallus became physician to King Charles IX. Not much more is known about Botallus, and history fails to record his date and place of death, as well as his image. The image depicted here is from his 1660 publication. Click on the image for a larger depiction.
Botallus' name is eponymically remembered in the following structures:
|
|
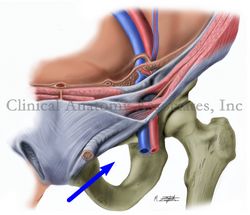
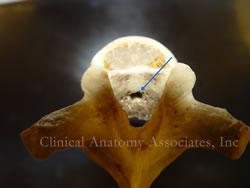
• Foramen of Botallus: The foramen ovale, an opening found in the fetus in the region of the fossa ovalis that closes upon birth
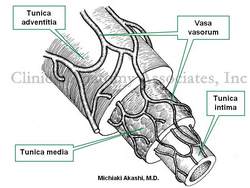
• Duct of Botallus: A communicating vessel between the left pulmonary artery and the proximal region of the descending aorta, part of fetal circulation, also known as the ductus arteriosus
• Ligament of Botallus: The closed ductus arteriosus in the adult
Sources:
1. "History of medicine; a correlative text, arranged according to subjects" Mettler, C Ch. 1947 The Blakiston Co
2. "Stedmans Medical Eponyms" Forbis, P; Bartolucci, SL. Williams & Wilkins 1998
3. "The origin of Medical Terms" Skinner, AH, 1970
4. "The First Closure of the Persistent Ductus Arteriosus" Alexi-Meskishvili,V; B?ttcher, W. Ann Thorac Surg 2010;90:349 –56
NOTE: There is no known image of Botallus. Skinner's "Origin of Medical Terms" shows one, but we could not confirm the origin of the image. If you know or have one, let us know!
|