I had the honor of being invited to participate in the 53rd Annual Chilean Meeting of Anatomy (XLIII Congreso Chileno de Anatomía) which was held in conjunction with the 1st Latin American Congress of Clinical Morphology (Primer Congreso Latinoamericano de Morfología Clínica). Along with these meetings were two symposia: The First Joint Symposium of Chilean/Korean Anatomists and the First Joint Chilean - IFAA-FIPAE Symposium (International Federation of Associations of Anatomists - Federative International Program for Anatomy Education).
Universidad de Los Andes, Chile
This meeting was held on November 11- 14, 2023 and was hosted by the University of Los Andes (Universidad de Los Andes), a Chilean institution of private higher education that offers careers and postgraduate programs in different areas of knowledge including Education, Engineering, Nursing, Obstetrics, Medicine, Psychology, Law. etc. Their campus is located on the slopes of the beautiful Andes mountains overlooking the city of Santiago, Chile.
The image shows the Main Library of the University, where the meeting was held.
On November 9 and 10, the days leading to the meeting, there were six Postgraduate Courses, from anatomy to radiology and surgical reconstruction. There were two that I would like to highlight. The first one was a workshop "Mastering Anatomical Radiology with IMAIOS", where one of the instructors was my good friend Dr. Cristian Uribe, who was one of the Meeting organizers. Dr. Uribe is one of the contributors to Medical Terminology Daily.
The second one was a "Workshop on Art & Science: A Theoretical-Practical Course on Anatomical Illustration". This course was directed by my good friend, Dr. Carlos Machado, world-renown medical illustrator, physician, and anatomist, editor of Netter's Atlas of Anatomy. Along with him two professors, Drs. Daniel Casanova and Valentina Cerda.
Nov. 11, 2023 Meeting opening
The Meeting was officially opened by Dr. Juan Carlos Lopez, Director of the Morphology Department of the Los Andes University. This was followed by a presentation on "The Role of the Placenta on the Modulation of Human Potential" by Dr. Sebastian Illanes. On the picture, from left to right, Dr. Jens Wasche (Germany), Dra. Valentina Cerda (Chile), Dr. Carlos Machado (Brazil/USA), me (Chile/USA), and Dr. Andres Riveros Valdes (Chile), a good friend and anatomist. Dr. Riveros is the President of the LatinAmerican Meeting on Clinical Morphology.
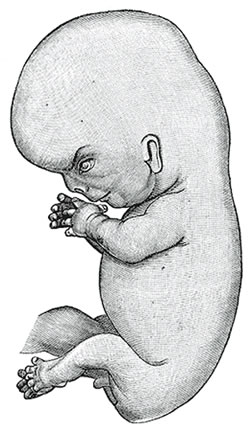
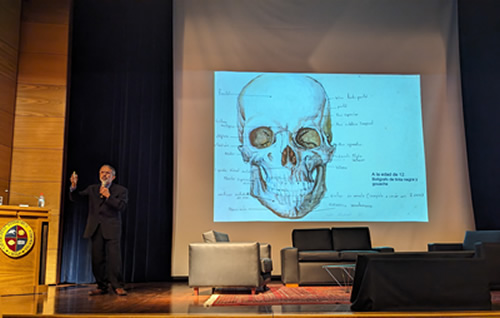
There were so many great presentations in this meeting! I think the attendees will agree with me that the conference by Dr. Carlos Machado on "The Art of Learning and Teaching Anatomy with Art" was one of the highlights of the Meeting. In his presentation Dr. Machado shared some of his early drawings and his career in Medicine and Medical Illustration, how he has used art to show patient pathology, and most important, the work and dedication that is required when developing a single image that will later become part of the Anatomy Atlases with which he collaborates.
Dr. Carlos Machado
The image above shows Dr. Machado during his presentation. On the screen an anatomical image he drew when he was 12 year old!.
Poster presentations during a coffee break
The meeting was also geared toward morphology students of different careers including Veterinary, Nursing, Dental School, and Medicine. The students presented their research posters during the coffee breaks. There were very high-quality and in-depth research, including the first osteology atlas of the Chilean flamingo (Phoenicopterus chilensis). I had interesting discussions on Latin terminology with these students.
There were extremely interesting topics throughout the week, including liver anatomy and liver transplant, ethics, philosophy, body donation, etc.
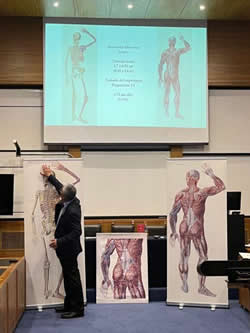
My presentation was based on the conference I delivered in May 2023 at the University of Antwerp, Belgium. Since the Belgium conference was delivered to a group of Andreas Vesalius experts, this one included much more information on Andreas Vesalius, his work, and additional information on printing techniques circa 1550.
Dr. Miranda during his presentation at the
XLIII Anatomy Meeting in Chile
The presentation added information on the history of the woodblocks used to print the 1543 Fabrica, the 1555 Fabrica, as well as other books that include the 1925 "The Iconography of Andreas Vesalius" by M.H. Spellman, and the 1934 Icones Anatomicæ.
The included picture was taken towards the end of my presentation where with the help of Dr. Uribe we unveiled Giovanni Paolo Mascagni's (1755-1815) work. At the center is a life-size copy of one of the pages of his book "Anatomiæ Universæ Icones", published in 9 installments between 1823 and 1832. It is important to note that each page of this book was hand-colored by Antonio Serantoni (1780-1837), thus the time it took to print and publish this book.
Mascagni's book, the largest book ever printed, shows in separate pages one third of a larger, life-size individual. Because of the rarity and value of this magnificent work, it cannot be cut and pasted.There are 16 know copies of Mascagni's anatomical opus magnus in the world, one of them at the University of Cincinnati, Ohio. USA.
With the help of Mr. Gino Pasi curator of the Henry Winkler Center for the History of the Health Professions, and the help of Mrs. Samantha Scheck, graphic designer, we measured and scanned some pages of the "Anatomiæ Universæ Icones", cleaned the background (no changes were done to the image itself) and pasted them digitally. The result is a life-size male 5.9 ft tall (1,75 mt). The images are incredible, and having traveled back and forth to Belgium and Chile, they are now part of my personal library.
Once again, my thanks to my old and new friends for making my stay so interesting, both personally and professionally. My thanks to the organizers of these meetings and symposia:
Dr. Juan Carlos López Navarro
President XLIII Chilean Anatomy Meeting
Director Morphology Department - Universidad de Los Andes
Dr. Andrés Riveros Valdés
President I Latin American Clinical Morphology Meeting
Professor - Universidad San Sebastián
Dra. Viviana Toro Ibacache
President Scientific Committee
Professor - Universidad de Chile
Dr. Emilio Farfán Cabello
President Chilean Anatomy Society
Professor - Pontificia Universidad Católica de Chile