How many scientists, physicians, or anatomists have musical pieces written for them? I was so surprised when I found out that there is a musical score entitled “André Vésale” written by Louis-Jean Abadie and published in 1861 in Paris, France. I felt the obligation to research this topic.
There are many people that follow the life and works of Andreas Vesalius, a 16th century anatomist who started the modern scientific approach to human anatomy and medicine. I count myself in this group that includes artists, historians, poets, painters,musicians, medical illustrators, physicians, surgeons, antique collectors, anatomists, etc.
In June 2023, I had the honor of being invited by the University of Antwerp in Belgium to speak at the 2023 Vesalius Triennial Meeting. It was here that I discovered this musical surprise!
One of the events of this meeting was an afternoon concert entitled “Vesalian landscapes in music, poetry, and photographs” by pianist Elke Robersscheuten, and my friend Theo Dirix, who read the poetry. This was accompanied by slides of Vesalian works, and images of the city of Brussels and the island of Zakynthos, Greece. One of the pieces performed by Elke Robersscheuten was “André Vésale”. You can see Elke perform this piece in a video at the end of this article.
With the help of Theo, I started the process of unraveling the story of this musical piece:
Louis Abadie
The author
Abadie, Louis-Jean (c1814-1858). Louis Abadie was a baritone singer. He started performing in the French provinces as member of an opera troupe. In 1842 he settled in Paris where he wrote numerous chansons and romances which were very popular at the Paris salons at the time. He had success as singer and voice teacher in Paris and in 1848 he released records of his songs, which were well received. I have not been able to find copies of these records.
He went back to traveling and singing, with little success and decided to move to Bordeaux, and then back to Paris where he was unsuccessful trying to find a locale that would present his work to the public. He lived in poverty and in early December 1958 he had a stroke and died at 45 years old, leaving a wife and three children. As a side note to his life, many of his works were dedicated or mentioned by name a woman named Jeanne. His wife's name was Marie Jeanne Toussaint.
Seven years after his death, on May 2, 1867, Les Danseurs de Corde.(The Rope Dancers) , an operetta (comedic opera) in two acts for which he had written the music, was performed at the Théâtre des Folies-Saint-Germain.
The lyrics
The poignant lyrics to this work were written by Louis-Adolphe Turpin de Sansay (1832 – 1891) a prolific French dramatic author, chansonnier, and songwriter. He collaborated with musicians with lyrics for their work. The lyrics for “André Vésale” were written in 1860 and published the following year.
The works of Turpin de Sansay were presented in elite places line the Théâtre des Champs-Élysées, the Théâtre des Bouffes-Parisiens, the Théâtre Beaumarchais, and the Théâtre-Lyrique.
The lyrics for “André Vésale” are based on Vesalius being deported to the Greek island of Zakynthos (known then as Zanthe). We now know this is a legend and not true. Following is the French original and a free translation of this work:
"André Vésale" (French)
Dans un caveau sur ma table de pierre
J'ai de la mort compulsé les secrets.
J'ai de mes mains profané la matière,
Et maintenant j'éprouve des regrets.
Par mon travail si de l'anatomie
J'ai découvert et promulgué la loi:
Si j'ai cherché les sources de la vie,
Pardonnez-moi, mon Dieu, pardonnez-moi!
Ils m'ont banni sur la terre de Zante,
Ils m'ont traité d'impie et d'imposteur;
Et j'ai dû tendre une main suppliante,
Car sur mon front plane le noir malheur!
Mais l'avenir, qui devant moi rayonne,
A ranimé mon courage et ma foi;
Si j'ai rêvé du martyr la couronne,
Pardonnez-moi, mon Dieu, pardonnez-moi!
J'aurais voulu calmer chaque souffrance,
Venir en aide à notre humanité,
Malgré l'exil, cependant, la science
Se répandra dans la postérité!
A mon pays, quoi qu'ingrat, je signale
Mes longs travaux, c'est mon bien, c'est mon droit.
Si j'illustrai le nom d'André Vésale,
Pardonnez-moi, mon Dieu, pardonnez-moi!
"Andreas Vesalius" (English)
In a cellar, on my stone table
I have extracted the secrets of death.
I have desecrated matter with my hands,
And now I feel regret.
By my work of anatomy
I discovered and promulgated the law:
If I sought the sources of life,
Forgive me, my God, forgive me!
They banished me to the land of Zakynthos,
They called me impious and impostor.
And I had to hold out a pleading hand,
For on my forehead hovers black misfortune!
But the future, which shines before me,
Revived my courage and my faith.
If I dreamed of the martyr's crown,
Forgive me, my God, forgive me!
I would have liked to calm each suffering,
Come to the aid of humanity,
Despite the exile, however, science
Will spread to posterity!
To my country, although ungrateful, I point out (that)
My vast work is my property, it is my right.
If I inscribe the name of Andreas Vesalius,
Forgive me, my God, forgive me!
The publisher
Étienne Challiot (1837 – 1866) had his office located at 352-354 Rue St Honoré, in Paris, very close to Place Vendôme, Paris. He published books and music sheets. Some of his publications can be found online.
The printer
Almost nothing is known about the printer of this work. A female printmaker, Madame Dinquel, had her printer shop at 276 Rue Sain Honoré, in Paris, very close to the publisher Étienne Challiot. Today, Sapporo, a Japanese restaurant sits at this address.
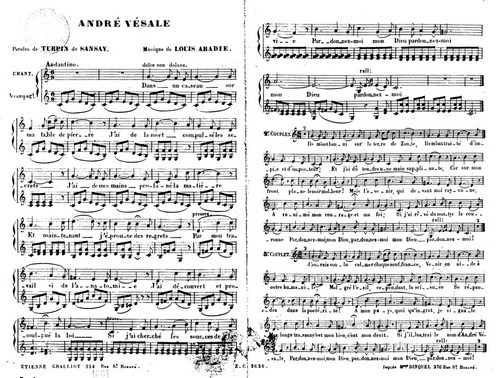
The musical piece
Following is a video of pianist Elke Robersscheuten performing "André Vésale" by Luis Abadie.
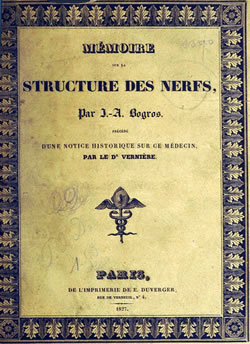
The original score can be
downloaded here. Thanks to
IMLSP for preserving this music for posterity. You can click on the image for a larger depiction.
André Vésale sheet music by Luis Abadie. Public Domain
Sources:
1. Biographie universelle des musiciens et bibliographie générale de la musique, Volume 1François-Joseph Fétis Libraire de Firmin-Didot, 1878 Paris
2. Obituary: Courrier de la librairie: journal de la propriété littéraire et artistique pour la France et pour l'étranger. 1858,7/12
3. Necrologie; B. JOUVIN. Théatres (French). Paris: Figaro, 09/12/1858. Article nécrologique dans Le Figaro (Lire en ligne sur Gallica)
4. Obituary: Courrier de la librairie: journal de la propriété littéraire et artistique pour la France et pour l'étranger. 1858,7/12
5. Frédéric Caille, La figure du sauveteur : Naissance du citoyen secoureur en France, 1780-1914, Presses Universitaires de Rennes, 2006, p. 222-224 6.